 In 2005 and 2006, the Ministry of Health and Long Term Care drastically overhauled their process for auditing physicians’ OHIP billing. The revised process, called the Payment Integrity program, is still in effect and is intended to ensure that physicians bill OHIP properly for their services. To expedite payment to physicians, the MOH processes claims on an ‘honour system’ after their computers run an initial – but not particularly thorough – check. But, as claims assessors and adjudicators have told us for years, payment of a claim does not necessarily mean that payment requirements have been met.
In 2005 and 2006, the Ministry of Health and Long Term Care drastically overhauled their process for auditing physicians’ OHIP billing. The revised process, called the Payment Integrity program, is still in effect and is intended to ensure that physicians bill OHIP properly for their services. To expedite payment to physicians, the MOH processes claims on an ‘honour system’ after their computers run an initial – but not particularly thorough – check. But, as claims assessors and adjudicators have told us for years, payment of a claim does not necessarily mean that payment requirements have been met.
Consequently, to make sure that OHIP funds are being used properly, OHIP has a post-payment review process. The ministry can engage in post-payment review for a variety of reasons, but reviews normally result from concerns raised by claims assessors who may notice something unusual or conflicts in medical billing across multiple physicians. For particularly problematic codes, the ministry can also conduct province wide reviews to analyze how billing codes are being used.
The first step in a post-payment review is typically educational. Individual education letters are sent directly to physicians explaining the potential concern and possibly requesting records of specific patients. These records are used to verify that the correct service was billed, and the ministry will determine if the physician has been billing properly.
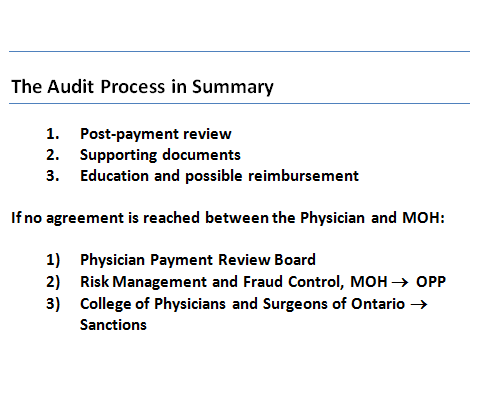
At this stage, the ministry will educate the physician, if necessary, on proper medical billing protocols. The MOH could also ask the physician to ‘pay back’ previously paid submissions. If the physician does not agree with the conclusions reached during the post-payment review, the disagreement will normally be escalated to the Physician Payment Review Board where both sides can make their arguments.
Finally, in the rare cases where a review of records or billing patterns suggests fraudulent billing activity, the Ministry can refer the case to the Risk Management and Fraud Control unit of the MOH. This body will determine if the case warrants forwarding to the OPP for criminal investigation. The ministry can also send the case to the College of Physicians and Surgeons of Ontario which could lead to sanctions and restrictions on the physician’s ability to practice.
As this post demonstrates, the Payment Review process is not something that should be feared by physicians. It’s meant to be educational, not confrontational. In next week’s post, we will explore the Payment Review process in action with a case study of one of JCL’s physicians.
